Cirrhosis Progression by Stage: Full Timeline
Understanding Cirrhosis: An Overview
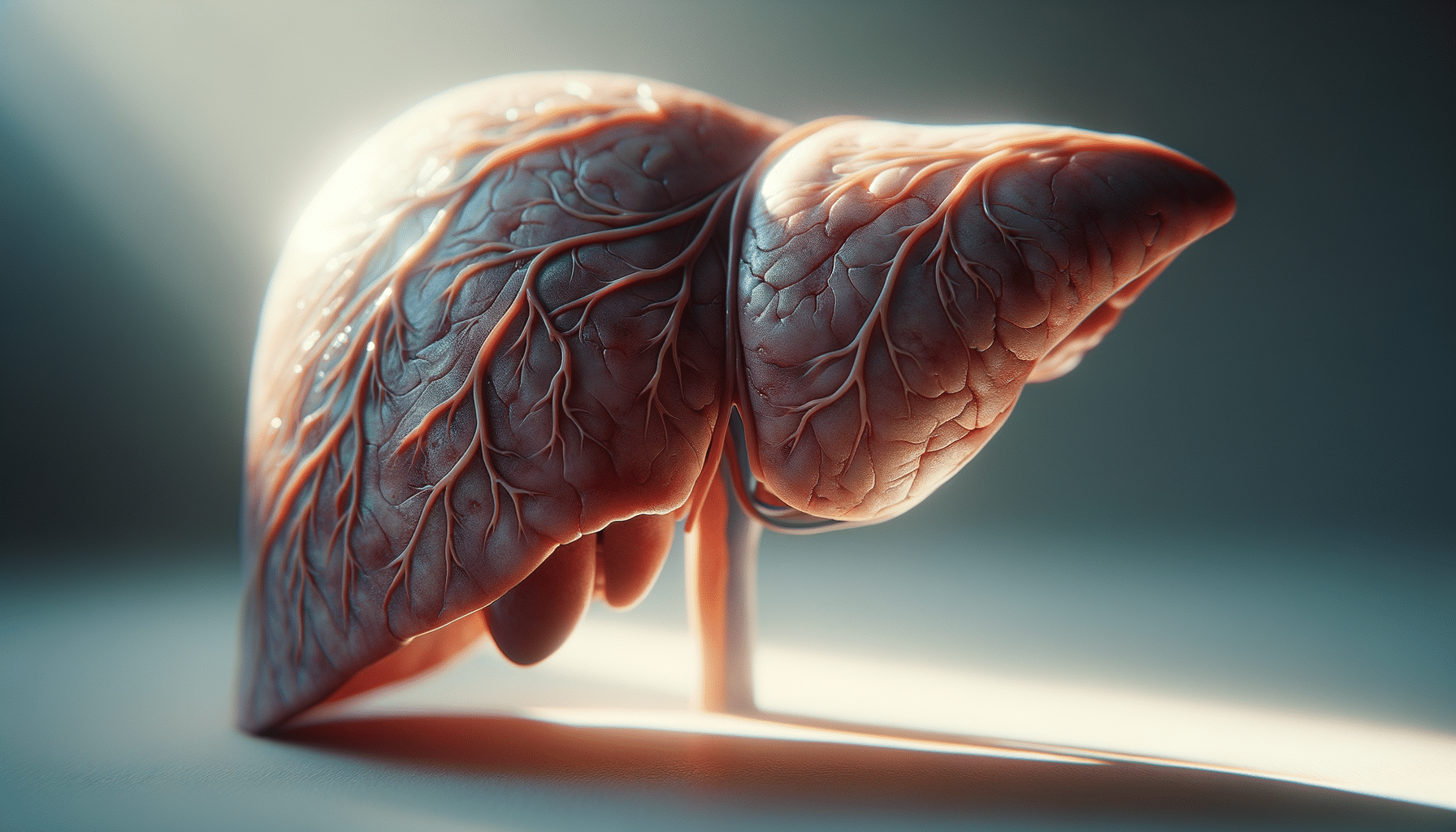
Cirrhosis is a chronic liver disease characterized by the gradual replacement of healthy liver tissue with scar tissue. This scarring disrupts the liver’s normal functions, such as detoxifying the blood, producing proteins necessary for blood clotting, and aiding in digestion. The progression of cirrhosis occurs in distinct stages, each with its own set of symptoms and implications for the patient’s health. Understanding these stages is crucial for managing the disease effectively and improving patient outcomes.
The liver is a resilient organ, capable of regenerating damaged cells. However, when the damage becomes extensive due to factors like chronic alcohol consumption, hepatitis, or fatty liver disease, the regenerative capacity is overwhelmed, leading to cirrhosis. Early diagnosis and intervention are key to slowing the progression and improving quality of life. Let’s delve into the stages of cirrhosis to better comprehend its impact on the liver and overall health.
Stage 1: Compensated Cirrhosis
In the initial stage of cirrhosis, known as compensated cirrhosis, the liver still manages to perform its essential functions despite the presence of scar tissue. At this stage, patients may not exhibit obvious symptoms, making early detection challenging. Routine liver function tests or imaging studies conducted for other reasons often reveal the condition.
During compensated cirrhosis, the liver compensates for the damage by working harder, which can delay the onset of symptoms. However, this stage is a crucial window for intervention. Lifestyle changes, such as abstaining from alcohol and managing underlying health conditions, can slow disease progression significantly.
Key characteristics of compensated cirrhosis include:
- Minimal or no symptoms
- Normal liver function tests
- Potential for stabilization with proper management
Early intervention can prevent further liver damage and improve life expectancy, highlighting the importance of regular health check-ups, especially for individuals at risk.
Stage 2: Decompensated Cirrhosis
As cirrhosis progresses to the decompensated stage, the liver’s ability to function effectively diminishes. This stage is marked by the onset of symptoms due to impaired liver function and complications arising from portal hypertension, a condition where increased blood pressure in the portal vein leads to various systemic issues.
Common symptoms and complications of decompensated cirrhosis include:
- Jaundice (yellowing of the skin and eyes)
- Ascites (accumulation of fluid in the abdomen)
- Hepatic encephalopathy (confusion and cognitive impairment)
- Variceal bleeding (bleeding from dilated veins in the esophagus or stomach)
At this stage, medical intervention becomes critical. Treatment focuses on managing symptoms, preventing complications, and preparing for potential liver transplantation. Regular monitoring and medications to reduce portal hypertension and manage fluid retention are common strategies.
Understanding the symptoms and seeking timely medical attention can significantly improve the quality of life for individuals with decompensated cirrhosis.
Stage 3: Advanced Cirrhosis
In advanced cirrhosis, the liver experiences extensive scarring, severely compromising its ability to function. This stage is characterized by frequent and severe complications, often leading to hospitalizations. Patients may experience a decline in their overall health and require extensive medical care.
Advanced cirrhosis is often accompanied by liver failure, where the liver can no longer perform its vital functions. Symptoms become more pronounced, and the risk of life-threatening complications increases. In addition to the symptoms seen in decompensated cirrhosis, patients might experience:
- Severe fatigue and weakness
- Significant weight loss and muscle wasting
- Increased susceptibility to infections
At this stage, liver transplantation may be considered as a treatment option. The evaluation for transplantation involves a thorough assessment of the patient’s overall health and the potential for successful recovery post-transplant. For those not eligible for transplantation, palliative care focuses on symptom management and improving quality of life.
Advanced cirrhosis underscores the importance of early detection and intervention in managing this progressive disease.
Stage 4: End-Stage Liver Disease (ESLD)
End-stage liver disease (ESLD) represents the final phase of cirrhosis, where the liver has sustained irreversible damage, and liver function is severely compromised. At this stage, the patient’s condition is critical, with multiple organ systems potentially affected by the liver’s inability to perform its functions.
ESLD is often characterized by the following:
- Severe jaundice and pruritus (itching)
- Persistent hepatic encephalopathy
- Recurrent ascites and variceal bleeding
- Renal dysfunction or failure
Patients with ESLD frequently require hospitalization and intensive medical care. Liver transplantation remains the definitive treatment, offering a chance for extended survival and improved quality of life. However, the availability of donor organs and the patient’s overall health can limit this option.
For patients not eligible for transplantation, managing symptoms and providing supportive care are the primary focus. This stage highlights the critical nature of early intervention and the need for comprehensive care strategies to support patients and families navigating this challenging phase of liver disease.


