Understanding the Progression of Cirrhosis
Introduction to Cirrhosis
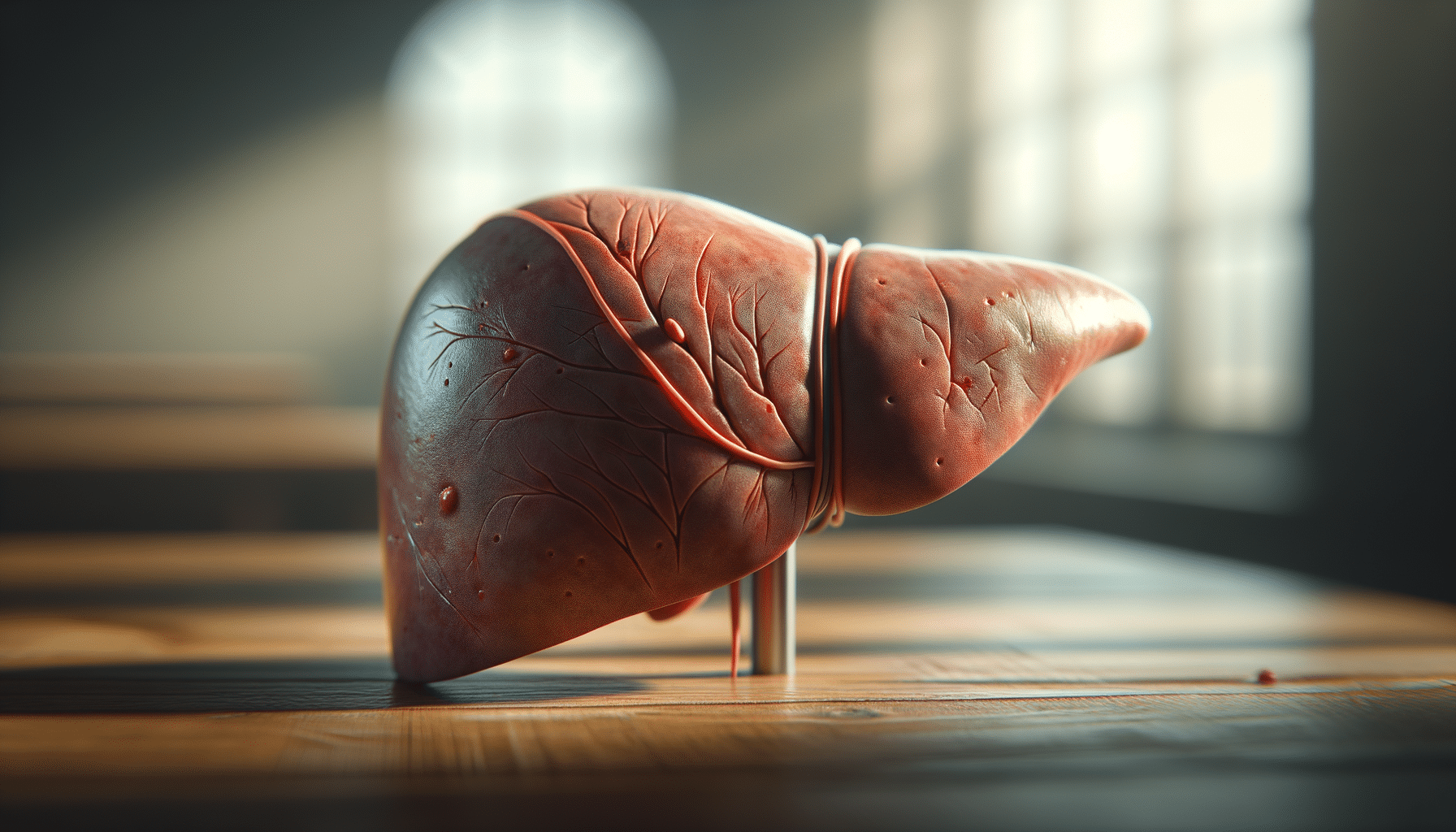
Cirrhosis is a chronic liver disease characterized by the replacement of healthy liver tissue with scar tissue, leading to a progressive decline in liver function. The liver, an essential organ in the body, is responsible for various functions including detoxification, synthesis of proteins, and production of biochemicals necessary for digestion. When cirrhosis occurs, these functions are impaired, which can lead to serious health complications. Understanding the progression of cirrhosis is crucial for managing the condition and improving patient outcomes.
The importance of early diagnosis and treatment cannot be overstated, as cirrhosis can lead to irreversible damage and life-threatening conditions such as liver failure or liver cancer. This article will delve into the causes, symptoms, treatment options, and the potential for reversing or stabilizing cirrhosis, offering valuable insights for those affected by this condition.
Causes and Risk Factors of Cirrhosis
Cirrhosis can develop from various underlying causes, each contributing to liver damage over time. One of the most common causes is chronic alcohol abuse, which leads to the accumulation of toxins and fat in the liver, eventually causing scarring. Another significant cause is hepatitis, particularly hepatitis B and C infections, which can lead to inflammation and gradual liver damage.
Other risk factors include:
- Nonalcoholic fatty liver disease (NAFLD), often associated with obesity and metabolic syndrome.
- Chronic viral infections, such as hepatitis D, which exacerbate liver damage.
- Genetic disorders, including hemochromatosis and Wilson’s disease, that affect the liver’s ability to function properly.
- Prolonged exposure to environmental toxins or certain medications that can harm the liver.
Understanding these causes and risk factors is essential for prevention and early intervention. Lifestyle modifications, such as reducing alcohol consumption and managing weight, can significantly decrease the risk of developing cirrhosis. Moreover, routine screening for hepatitis and other liver-related conditions can aid in early detection and treatment, potentially halting the progression of liver damage.
Symptoms and Diagnosis of Cirrhosis
The symptoms of cirrhosis often develop gradually and may not be noticeable in the early stages. As the disease progresses, symptoms become more pronounced and can include fatigue, jaundice (yellowing of the skin and eyes), and swelling in the legs and abdomen. Patients may also experience easy bruising, confusion, and spider-like blood vessels on the skin.
Diagnosing cirrhosis typically involves a combination of medical history, physical examination, blood tests, imaging studies, and sometimes a liver biopsy. Blood tests can reveal liver function abnormalities, while imaging studies such as ultrasound, CT scans, or MRI can provide detailed visuals of the liver structure to assess the extent of scarring.
Early diagnosis is crucial for managing cirrhosis effectively. It allows healthcare providers to implement treatment strategies that can slow the progression of the disease and improve quality of life. Regular monitoring and follow-up are essential parts of managing cirrhosis, helping to detect complications early and adjust treatment plans as needed.
Treatment Options for Cirrhosis
Treatment for cirrhosis focuses on slowing the progression of liver damage, preventing complications, and addressing the underlying cause of the disease. Lifestyle changes are often a fundamental part of treatment, including abstaining from alcohol, following a healthy diet, and maintaining a healthy weight.
Medications can also play a role in managing cirrhosis:
- Antiviral drugs for hepatitis B and C can reduce liver inflammation and prevent further damage.
- Medications to control symptoms such as itching, fatigue, and fluid retention.
- Newer medications are being developed to target specific pathways involved in liver fibrosis, offering hope for slowing or reversing the progression of cirrhosis.
In severe cases, where liver function is significantly impaired, a liver transplant may be considered. This option involves replacing the diseased liver with a healthy one from a donor. Liver transplantation can be life-saving, but it also involves rigorous evaluation and a commitment to lifelong medical care and medication.
Future Directions and Conclusion
Research into cirrhosis continues to evolve, with scientists exploring novel therapies and interventions that could improve outcomes for patients. One area of interest is the potential for regenerating liver tissue and reversing fibrosis, which could transform the management of cirrhosis in the future.
In conclusion, while cirrhosis is a serious and potentially life-threatening condition, understanding its progression and management can significantly improve patient outcomes. Early diagnosis, lifestyle modifications, and adherence to treatment plans are vital components in managing cirrhosis effectively. As research advances, there is hope for new treatments that could slow, halt, or even reverse the progression of this challenging disease.
By staying informed and proactive in their healthcare, patients with cirrhosis can work alongside their medical providers to manage their condition and maintain their quality of life.


